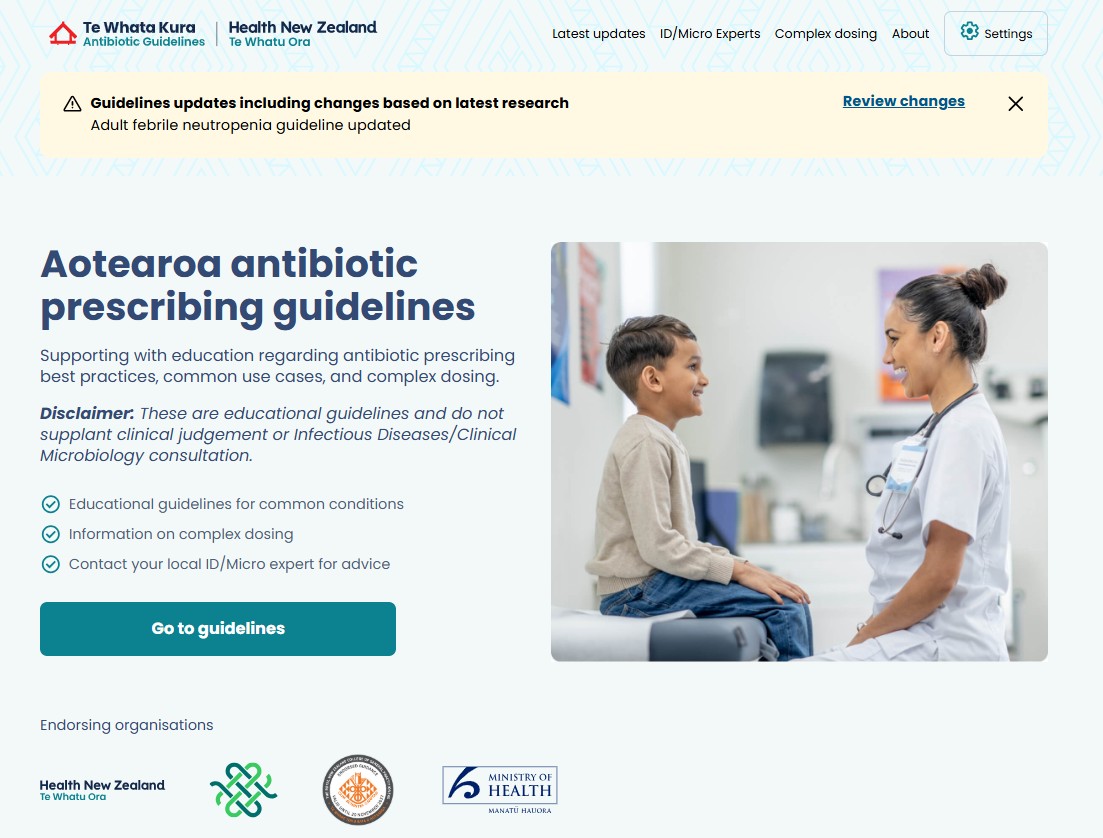
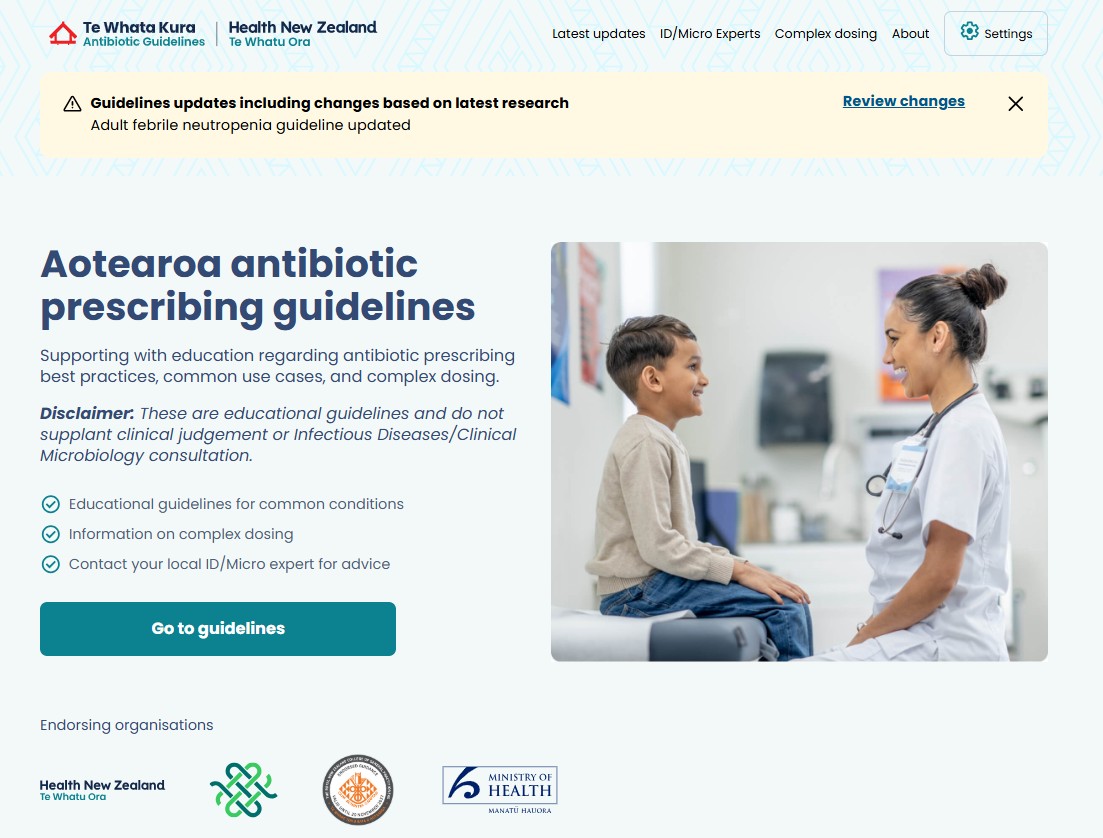
Te Whata Kura: Transforming Antibiotic Prescribing in Aotearoa
Te Whata Kura is a new national digital antibiotic prescribing guideline designed to tackle antimicrobial resistance and inconsistent prescribing practices across Aotearoa New Zealand.
Developed through a collaboration between clinical leaders, researchers and Health New Zealand, it provides nationally aligned, evidence-based decision support at the point of care. By integrating existing guidance into a single, accessible platform, it supports equitable, high-quality antibiotic stewardship across primary and secondary care. Enabled by UniServices through funding and partnership support, the initiative demonstrates how research and digital innovation can deliver system-wide health impact.
Te Whata Kura is a new national antibiotic prescribing guideline and digital decision support tool designed to address this challenge at scale, bringing together clinical leadership, digital innovation, and a commitment to equity in healthcare delivery.
The initiative showcases how national collaboration, bringing together researchers and clinicians from the University of Auckland’s Faculty of Medical and Health Sciences (FMHS), the University of Otago, Health New Zealand | Te Whatu Ora, and representatives from primary care across Aotearoa to drive system-level change that improves human health and wellbeing.
The challenge
New Zealand’s antibiotic prescribing landscape is fragmented. Prescribers in primary and secondary care have relied on a wide range of regional and specialty-specific guidelines, many of which differ in scope, clinical recommendations, and update frequency. This fragmentation has created several challenges:
- Inconsistent prescribing advice across regions and care settings
- Barriers to auditing and improving prescribing quality at a national level
- Difficulty supporting prescribers who move between regions
- Limited ability to address inequities in antibiotic use and infectious disease outcomes
At the same time, New Zealand faces some of the highest rates of antibiotic resistance in the developed world, including methicillin-resistant Staphylococcus aureus (MRSA), amoxicillin-resistant Escherichia coli, and reduced penicillin susceptibility in Streptococcus pneumoniae. Seasonal spikes in antibiotic use, particularly for upper respiratory tract infections, come with inappropriate prescribing across all population groups.
This fragmentation has important equity implications and creates a powerful opportunity to embed consistent, high-quality antibiotic stewardship that can deliver substantial benefits for Māori and Pacific communities through improved, nationally aligned prescribing practice.
The solution to support prescribers: Te Whata Kura
Te Whata Kura, named to reflect antibiotics as a taonga (precious resource) and the guideline as a repository of shared knowledge, is a comprehensive national antibiotic guideline delivered through an intuitive digital platform. Its design is grounded in the principles of antimicrobial stewardship, recognising that using antibiotics as wisely as possible is essential to ensure these vital medicines remain effective for future generations of New Zealanders.
Accessible via a web browser and downloadable for offline use on mobile devices, Te Whata Kura provides patient-specific prescribing advice for all common infections across:
- Infants, children, and adults
- Patients with penicillin allergy
- Sepsis and severe illness
- Patients with prior MRSA infection
The guideline integrates and aligns advice from existing high-quality sources, including sexual health and rheumatic fever guidelines, into a single, nationally consistent decision support system.
Digital design and development were led by RUSH Digital (link), ensuring the platform is clinically robust, easy to navigate, and usable across diverse care settings, from urban hospitals to remote primary care clinics.
Research excellence, collaboration, and clinical leadership
Development of Te Whata Kura was funded by Te Niwha, the national infectious diseases platform (link), and led by a multidisciplinary national team anchored by FMHS researchers and clinicians from the University of Auckland.
The broader project team included:
- General practitioners
- Paediatric and adult infectious disease physicians
- Microbiology, immunology, pharmacy, and public health experts
- Nursing leadership
Contributors were drawn from across Aotearoa, including Tāmaki Makaurau, Te Whanganui-a-Tara, Ōtautahi, and Ōtepoti, ensuring broad clinical and regional representation.
The project is supported by Te Whatu Ora | Health New Zealand, PHARMAC, and NZ Formulary, aligning the guideline with national medicines policy and health system priorities.
An initial draft guideline was developed by synthesising existing national and international antibiotic guidance, then refined through extensive expert review. Decision algorithms were rigorously tested, and an early release in October 2025 enabled wide consultation with clinicians, specialty groups, and organisations. Feedback, particularly on approaches that promote equitable antibiotic use, was actively incorporated ahead of final publication in December 2025.
Clinical impact in practice
Te Whata Kura is designed to support prescribers at the point of care, including in complex clinical scenarios. For example:
- Community-based management of a child with extensive impetigo and prior MRSA infection
- Hospital-based treatment of pyelonephritis in a patient with chronic kidney disease
In some cases, the guideline challenges entrenched prescribing habits. One notable example is the recommendation not to prescribe antibiotics for most sore throats in patients who are not at increased risk of acute rheumatic fever, consistent with international evidence and guidelines from the UK, US, and Australia.
In most situations, however, prescribers are expected to find that recommendations closely align with best practice, now delivered through a single, trusted national source.
The project team is now working with Health New Zealand to establish ongoing governance and long-term maintenance arrangements. Formal endorsement has been approved, with implementation details currently being finalised. Importantly, the platform’s digital architecture allows content updates to be made without the need for hard-coding expertise, enabling rapid, dynamic changes in response to new evidence, emerging resistance patterns, or policy shifts.
Outcomes and future impact
Te Whata Kura establishes, for the first time, a nationally consistent approach to antibiotic prescribing that supports shared learning and best practice across primary and secondary care. This capability is expected to help:
- Reduce inappropriate antibiotic use
- Support targeted improvements in prescribing equity
- Improve outcomes for underserved populations
- Slow the growth of antimicrobial resistance nationwide
- Facilitate examination of antibiotic use in different settings in Aotearoa to identify opportunities to improve the equity and quality of antibiotic use
By making the same expert advice available to every prescriber, from Kaitaia to Rakiura, Te Whata Kura represents a step-change in how clinical knowledge is translated into practice.
Enabling impact through UniServices
UniServices played an enabling role, supporting engagement with Te Niwha and assisting with the practical funding and contractual processes that allowed Te Whata Kura to move from a research-driven idea toward a nationally supported health system initiative.
“UniServices helped make this work possible by connecting us with Te Niwha and supporting the negotiation process to bring Te Whata Kura into the Te Niwha funding programme. That support was critical in enabling us to scale this initiative and deliver impact nationally.”
— Steve Ritchie, Project Co-Lead Researcher, Faculty of Medical and Health Sciences, University of Auckland
This support reflects UniServices’ role in helping University of Auckland researchers navigate funding pathways, partnerships, and commercial and contractual processes, allowing clinical experts to focus on delivering research that improves health outcomes.
Research capability improving human health and wellbeing
Te Whata Kura shows how research excellence, digital delivery and system partnerships, can create scalable national impact - clinical expertise and great ideas becoming practical real-world solutions that improve human health and wellbeing.